
By Scott McGeary, DPT, CSCS and Stuart Helster, SPT, Hershey Center

Scott McGeary, DPT, CSCS
I will never forget the summer I trained for my first year of college cross country. In high school, I had been running about 35 miles during a high mileage week, but I wanted to hit 70 miles per week before my first day at Duquesne University. As many less experienced runners figure out the hard way, increasing mileage too quickly without proper flexibility and strength typically leads to an injury. By August, I started feeling a little ache in the outside of my knee. Within 1-2 weeks of that first feeling, the ache turned to pain. Eventually, it worsened to the extent where my knee locked up while running, and I had to walk home 1.5 miles (the absolute worst feeling for a runner). Fortunately, I worked as a physical therapy technician for Drayer Physical Therapy, so I immediately began treatment. The whole episode set me back about a month, which was detrimental to my first season. This was my first experience with IT Band Syndrome.
The iliotibial band (ITB) is a thick piece of leathery, dense tissue that begins as part of the gluteus maximus (buttocks) and tensor fascia latae (TFL) muscle tendons, runs along the outside of the thigh, traverses the widest part of the lateral epicondyle (knee), and inserts into the tibia (leg bone, below knee).
The problem is not typically the ITB itself, but rather faulty leg mechanics and tightness in the TFL and gluteus maximus.
Simply put, this manifests as knees collapsing inward during squats, lunges or running. This movement allows the ITB to rub over the lateral epicondyle of the femur (knee) and/or the greater trochanter of the hip, causing pain and inflammation at the site of friction.
Having these characteristics means a much higher likelihood of developing ITB Syndrome (ITBS).1 Most runners experience pain or discomfort at the knee, but plenty of them feel symptoms in the outside hip.
NSAIDS, deep friction massage, and steroid injections have limited effect on ITBS by themselves.2 Restoring proper mechanics and strengthening the hips and core can reduce pain and improve overall running efficiency. 3
Most likely, the gluteal muscles and hip external rotators are weak and not firing properly, which allows the hips to drop and knees to get too close or even smack together.
Performing a few key exercises can activate the involved muscles properly and build strength, which will reduce femoral internal rotation and knee collapse, thus reducing ITBS symptoms.
We recommend two stretches (one for each muscle), performed three to four times daily when the muscles are truly tight. After six weeks of this, stretching typically can be scaled back to just after runs or workouts. Patients should feel each stretch in the area of the targeted muscle.
While doing your table/floor exercises, always feel your buttocks to make sure you are activating the right area. While doing squats, lunges and jumping exercises, make sure your knees do not collapse inward or go forward past your toes.
3 sets of 10 reps for each exercise should be performed every other day.

Sidelying Hip Abduction

Bridges
If you’ve been beating up and overusing your TFL muscle, it likely has become too tight and needs to be stretched properly. Each of these stretches should be performed daily, three times each for 20 seconds.
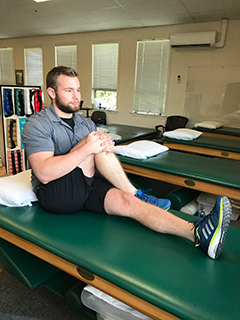
Seated IT Band Stretch

Standing IT Band Stretch
Symptoms lasting for a few weeks or just started to have pain but cannot figure out how to activate the proper muscles, then consider consulting a physical therapist for an evaluation of your mechanics and a specific program for your needs.
Drayer can treat most people via direct access (no prescription needed) for 30 days. A healthcare provider who specializes in running will know the rigors of training and mental/emotional stressors associated with not being able to train when injured.
To schedule an appointment, please contact a physical therapy location near you.


